Find Help
More Items From Ergsy search
-

Prolapse Management
Relevance: 100%
-

Prolapse Types and Tips
Relevance: 72%
-

Pelvic health: prolapse
Relevance: 71%
-

Pelvic health: prolapse
Relevance: 70%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 66%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 65%
-

How to manage type 2 diabetes
Relevance: 25%
-
Your pelvic health matters: insights from NHS clinicians
Relevance: 24%
-

Long COVID - Managing Breathlessness
Relevance: 24%
-

Is there a protocol for managing concussions in rugby?
Relevance: 24%
-

Can fiber help with weight management?
Relevance: 23%
-

Are there self-help strategies for managing health-related anxiety?
Relevance: 23%
-

Can fiber help with weight management?
Relevance: 23%
-

Managing Chronic Illness Within the Family
Relevance: 23%
-

How are food allergies managed in UK schools?
Relevance: 23%
-

Is Wegovy used for type 2 diabetes management?
Relevance: 22%
-

Understanding and Managing Respiratory Illnesses in Families
Relevance: 22%
-

Strategies for Managing Seasonal Affective Disorder
Relevance: 22%
-

Can lifestyle changes help manage ADHD?
Relevance: 22%
-

What is the role of pain management in treating whiplash?
Relevance: 22%
-

How can nut allergies be managed?
Relevance: 22%
-

Can stress management aid in menopause masking?
Relevance: 22%
-
What is the role of diet in managing heart failure?
Relevance: 22%
-

Can lifestyle changes help manage tinnitus?
Relevance: 22%
-

How are product recalls managed in the UK?
Relevance: 22%
-

Are there apps that help manage and reduce household bills?
Relevance: 22%
-
How can I manage pain after a C-section?
Relevance: 22%
-

Managing and treating your child's eczema
Relevance: 22%
-

What role do schools play in managing concussions?
Relevance: 22%
-

What are the qualifications of the staff managing virtual wards?
Relevance: 22%
-

Is there an NHS app for managing prostate cancer care?
Relevance: 22%
-

How do live-in caregivers manage their personal time?
Relevance: 21%
-

What is the role of potassium in managing blood pressure?
Relevance: 21%
-

Are there any NHS apps for managing menopause symptoms?
Relevance: 21%
-

What role do lifestyle changes play in managing psoriasis?
Relevance: 21%
-

Where can I find support for managing Type 2 Diabetes in the UK?
Relevance: 21%
-
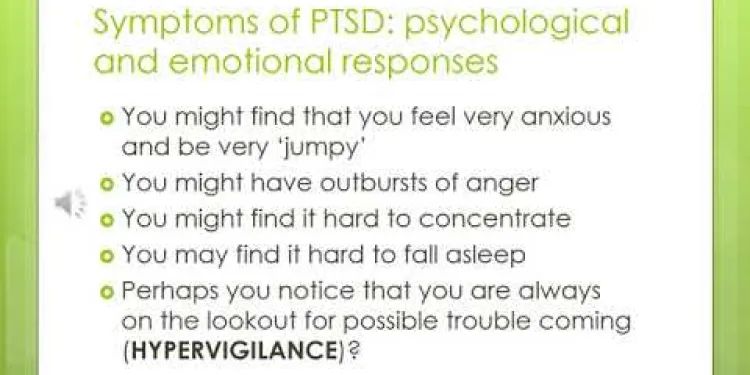
Understanding and Managing PTSD powerpoint slides with audio
Relevance: 21%
-

How important is the WHO for managing global pandemics?
Relevance: 21%
-

How can stress management affect cortisol levels?
Relevance: 21%
-

What role does diet play in managing obesity?
Relevance: 21%
Prolapse Management: A Comprehensive Guide
Understanding Prolapse
Prolapse occurs when pelvic organs, such as the bladder, uterus, or rectum, move from their normal position and descend into or outside of the vaginal canal. This condition is commonly associated with childbirth, obesity, menopause, and heavy lifting. While prolapse is not life-threatening, it can cause discomfort and inconvenience, impacting your quality of life.Symptoms of Prolapse
Signs of prolapse may vary depending on the organ involved but generally include a bulging sensation in the vagina, pelvic pressure, urinary incontinence, and difficulty with bowel movements. It might be recommended to consult a healthcare provider for a thorough evaluation if you experience any of these symptoms.Non-Surgical Management
For many individuals, non-surgical options can effectively manage prolapse. Pelvic floor exercises, commonly known as Kegel exercises, can strengthen the muscles that support the pelvic organs. Lifestyle modifications, such as losing weight and avoiding heavy lifting, can also contribute to managing the condition. Pessaries, which are medical devices inserted into the vagina, can provide physical support to the prolapsed organs.Surgical Options
If non-surgical treatments are ineffective or the prolapse is severe, surgical intervention might be necessary. Various surgical options are available, tailored to the specific type and severity of the prolapse. These surgeries aim to repair the prolapsed organ and restore normal anatomy. Minimally invasive techniques, such as laparoscopic surgery, often result in faster recovery times and reduced complications.Living with Prolapse
Living with prolapse can be challenging, but early intervention and appropriate management can significantly improve the quality of life. In the UK, numerous resources are available, including support groups, physiotherapy services, and specialized clinics. NHS websites and local health authorities can provide valuable information and guidance on accessing these services.When to Seek Medical Advice
While occasional mild symptoms might not be alarming, persistent or worsening symptoms warrant medical attention. It is essential to consult a healthcare provider to discuss symptoms, treatment options, and preventive measures. Early diagnosis and management can prevent further complications and enhance the effectiveness of treatment. In conclusion, prolapse management encompasses a range of non-surgical and surgical treatments aimed at alleviating symptoms and improving quality of life. Residents in the United Kingdom have access to numerous healthcare resources to manage this condition effectively. Always seek professional advice to determine the best course of action for your specific situation.Prolapse Management: A Comprehensive Guide
Understanding Prolapse
Prolapse happens when parts inside the body, like the bladder or uterus, move down from where they normally are. They might press into or come out of the vagina. This can happen after having a baby, gaining a lot of weight, going through menopause, or lifting heavy things. Prolapse is not dangerous, but it can be uncomfortable and make life harder.Symptoms of Prolapse
You might feel a bulge in your vagina or pressure in your pelvis. You might also have trouble holding in urine or have problems going to the bathroom. If you notice any of these signs, it's a good idea to talk to a doctor.Non-Surgical Management
Many people can feel better without surgery. Doing exercises called Kegels can make the muscles that hold up your organs stronger. Losing weight and not lifting heavy things might help too. Some people use a device called a pessary, which goes inside the vagina to hold things in place.Surgical Options
If other treatments don’t work or if the prolapse is bad, surgery might help. There are different surgeries depending on what you need. These surgeries fix the prolapse and help return things to normal. Some surgeries are done with small cuts, which can mean you heal faster.Living with Prolapse
Dealing with prolapse can be hard, but getting help early can make things better. In the UK, there are plenty of resources, like support groups and special clinics, to help you. Websites and local health services can give you information on how to get support.When to Seek Medical Advice
If you have symptoms that don’t go away or get worse, it’s important to see a doctor. They can help you understand your options for treatment and ways to prevent problems. Getting help early can make treatments work better. To sum up, there are many ways to manage prolapse, including treatments without surgery and surgeries. People in the UK can get a lot of help from healthcare services. Always talk to a doctor to find out what’s best for you.Frequently Asked Questions
What is pelvic organ prolapse?
Pelvic organ prolapse is a condition where one or more of the pelvic organs, such as the bladder, uterus, or rectum, descends from its normal position.
What are the common symptoms of prolapse?
Common symptoms include a feeling of pressure or fullness in the pelvic area, urinary incontinence, difficulty with bowel movements, and lower back pain.
Who is at risk for developing a prolapse?
Women are at higher risk, particularly those who have given birth, are postmenopausal, or have undergone previous pelvic surgery. Obesity and heavy lifting can also increase risk.
How is a prolapse diagnosed?
A prolapse is typically diagnosed through a physical examination by a GP or gynaecologist. Additional tests, such as ultrasound or MRI, may be performed for further evaluation.
What non-surgical treatments are available for prolapse?
Non-surgical treatments include pelvic floor exercises, lifestyle changes, like weight loss and avoiding heavy lifting, and the use of pessaries to provide support.
What is a pessary?
A pessary is a silicone device inserted into the vagina to provide support and alleviate symptoms of pelvic organ prolapse. It is usually fitted and prescribed by a healthcare professional.
When is surgery recommended for prolapse?
Surgery is recommended when non-surgical treatments are ineffective, or the prolapse is severe. Surgical options can include vaginal repairs, hysterectomy, or mesh implants.
What are the risks of prolapse surgery?
Potential risks include infection, bleeding, pain, urinary or bowel issues, and recurrence of the prolapse. Discussing these risks with a surgeon is essential.
Can lifestyle changes help manage prolapse?
Yes, maintaining a healthy weight, avoiding heavy lifting, doing pelvic floor exercises, and eating a high-fibre diet to prevent constipation can help manage prolapse symptoms.
What are pelvic floor exercises?
Pelvic floor exercises, or Kegels, involve contracting and relaxing the pelvic floor muscles to strengthen them. This can help manage and prevent prolapse symptoms.
How long does recovery take after prolapse surgery?
Recovery times can vary, but it typically takes 6-12 weeks to heal fully. Patients should avoid heavy lifting and strenuous activities during the recovery period.
Is it possible for a prolapse to recur after treatment?
Yes, there is a possibility of prolapse recurrence after treatment, especially if underlying risk factors are not addressed. Regular follow-up with a healthcare provider is crucial.
Are there any complications if a prolapse is left untreated?
Untreated prolapse can lead to complications such as urinary difficulties, bowel issues, and discomfort, which can significantly impact quality of life.
Can men experience pelvic organ prolapse?
While rare, men can experience a form of pelvic organ prolapse, such as rectal prolapse, where part of the rectum protrudes through the anus.
Where can I find support for managing prolapse?
Support can be found through healthcare providers, pelvic health physiotherapists, and organisations such as the Pelvic Organ Prolapse Support Association (POPSA) in the UK.
What is pelvic organ prolapse?
Pelvic organ prolapse is when organs in the lower belly, like the bladder, move from where they should be. They might push against the muscles of the belly.
This can happen because the muscles are weak or stretched.
If you need help to understand or read, you can:
- Ask a friend or family member to explain.
- Use text-to-speech tools to listen to the information.
- Look at pictures or videos that show what is happening in the body.
Pelvic organ prolapse happens when a part inside your belly, like the bladder, womb, or rectum, moves down from where it should be.
What are the common signs of prolapse?
Here are some signs that might mean someone has a prolapse:
- A feeling of heaviness or pressure in the lower belly.
- Feeling like a lump or bulge is coming out of the vagina or back passage.
- Having trouble peeing or emptying the bowels.
- Back pain or feeling uncomfortable.
If you or someone you know has these signs, it is a good idea to talk to a doctor.
To help understand, you can:
- Ask someone you trust to read it with you.
- Use a picture of the body to point where it hurts.
- Write down questions to ask the doctor.
Some signs you might notice are a tight or full feeling in your tummy, trouble holding in your pee, finding it hard to poo, and pain in your lower back.
Who can get a prolapse?
Women are more at risk. Women who have had babies, are older, or have had pelvic surgery are at higher risk. Being overweight and lifting heavy things can also make the risk higher.
How do doctors know if you have a prolapse?
A prolapse is when something inside the body moves out of place. A doctor can find out if you have a prolapse by checking your body. This is called a physical check. Sometimes, doctors use special cameras like an ultrasound or MRI to take pictures inside your body. This helps them learn more about the prolapse.
What are the treatments for prolapse that do not need surgery?
There are some ways to help prolapse without having an operation.
- Exercises: Doing special exercises, like pelvic floor exercises, can make the muscles stronger.
- Diet and Lifestyle: Eating healthy food and staying at a healthy weight can help.
- Devices: A device called a pessary can be placed inside to give support.
If you need help or have questions, it is good to talk to a doctor or nurse. They can help you find the best way to feel better.
There are ways to help that don’t need surgery. You can try exercises to make your pelvic floor muscles stronger. You might also want to change some things in your life. Losing weight can help, and it’s good to not lift heavy things. Some people use special devices called pessaries that give support.
What is a pessary?
A pessary is a small device. It is put inside the body. It helps support areas like the bladder or womb. If you are not sure about it, you can ask a doctor or nurse to help explain.
If reading is hard, you can use tools like audiobooks or get someone to read aloud for you. Drawing pictures can also help you understand better.
A pessary is a soft, rubber-like ring that goes inside the vagina. It helps hold things up in the body and makes some health problems better. A doctor or nurse usually helps you get the right size and puts it in for you.
When do doctors say to have an operation for prolapse?
Sometimes a part inside your body, like the bladder or womb, moves out of place. This is called a prolapse.
Doctors might say you need an operation to fix it if:
- You feel very uncomfortable or in pain.
- It is hard for you to pee or poop.
- You have trouble doing everyday things.
If you think you have prolapse, talk to your doctor. They can help you decide what to do.
Tools that can help you:
- Pictures or diagrams to show what happens in the body.
- Simple words or videos to explain prolapse.
Doctors suggest surgery if other treatments don’t work, or if the prolapse is very bad. Surgery can mean fixing it through the vagina, taking out the womb, or using a special mesh.
What can happen after prolapse surgery?
If you have surgery, some things can go wrong. Here is what might happen:
- There might be pain.
- The place where you had surgery could get infected and you could feel sick.
- You might have trouble going to the bathroom.
- The surgery might not fix the problem, and you might need more help.
- Some people might feel problems when peeing or pooping.
Before having surgery, ask your doctor questions. Make sure you know what might happen. It's good to have someone with you, like a friend or family member, to help you understand.
Using pictures or videos can also help you understand more about the surgery.
There are some risks you should know about. You could get an infection, have bleeding, feel pain, or have problems with peeing or pooping. The prolapse might also come back. It's important to talk to the doctor about these risks.
Can changing how you live help with prolapse?
Changing how you live might help with prolapse. Prolapse is when something inside the body moves out of place. Here are some simple things that might help:
- Exercise: Try gentle exercises like walking or swimming. Ask a doctor about special exercises you can do.
- Healthy Eating: Eat lots of fruits and vegetables. Drink plenty of water.
- Avoid Heavy Lifting: Do not lift heavy things. This can make prolapse worse.
- Rest: Make sure you get enough sleep and rest during the day.
Talking to a doctor or nurse can help. They can give you more advice. You can also ask a family member or friend to help you with these changes.
Yes, staying at a healthy weight, not lifting heavy things, doing special exercises for your pelvic floor, and eating foods with lots of fiber to avoid constipation can help with prolapse symptoms.
What are pelvic floor exercises?
Pelvic floor exercises help make the muscles in your lower tummy (belly) strong.
These exercises are good for your body. They can help you stop leaks when you laugh or sneeze.
It is easy to do these exercises at home.
To do them, squeeze the muscles you use to stop a wee (pee). Hold for a few seconds, then let go.
Repeat a few times each day to get better at it.
You can ask a doctor or nurse for help if you need it. They can show you how it’s done.
Pelvic floor exercises, or Kegels, are movements to make your pelvic floor muscles stronger. You can do this by squeezing and relaxing these muscles. These exercises can help stop problems from happening or getting worse.
How long does it take to get better after prolapse surgery?
It can take a few weeks to start feeling better after prolapse surgery. Everyone is different, so some people might take more time.
Here are some tips to help you recover:
- Rest a lot and do not lift heavy things.
- Eat healthy foods like fruits and vegetables.
- Ask someone to help you with daily tasks.
- Talk to your doctor if you have questions or feel pain.
Using these tips can help you heal well and feel good again.
It can take 6 to 12 weeks to get better. During this time, don't lift heavy things or do hard activities. Take it easy while you heal.
Can a prolapse happen again after it has been treated?
A prolapse is when something inside the body slips out of place. After it is fixed, sometimes it might happen again.
Tools and techniques that might help:
- Talk to your doctor about ways to stop it from happening again.
- Do special exercises to make your body stronger.
- Use pictures or videos to learn more about prolapses.
Yes, the problem can come back after treatment. This might happen if the main causes are not fixed. It is very important to see a doctor regularly.
What happens if a prolapse is not treated?
If you do not treat a prolapse, it can cause problems later. Your organs might not work right. It can make you feel hurt or uncomfortable.
Here are some tips to help:
- Talk to a doctor or nurse. They can help you understand what to do.
- Use pictures or diagrams. They can help you learn more easily.
- Ask a family member or friend to explain things. They can help you feel better.
If prolapse is not treated, it can cause problems. These problems might include trouble peeing, trouble with pooping, and feeling uncomfortable. These issues can make life a lot harder.
Can men have pelvic organ problems?
It is not very common, but sometimes men can have a problem called rectal prolapse. This is when part of the rectum (a part of the body that helps with going to the bathroom) sticks out through the bottom (anus).
Where can I get help for prolapse?
If you need help with prolapse, there are places that can support you. Here is where you can look:
- Doctors: Talk to your doctor. They can give you advice and treatments.
- Nurses: Nurses in clinics or hospitals can help you understand prolapse and how to manage it.
- Online Support Groups: You can join groups online where people talk about living with prolapse.
If reading is hard, you can try using voice tools that read texts aloud for you, like screen readers.
You can get help from doctors, special therapists for pelvic health, and groups like the Pelvic Organ Prolapse Support Association (POPSA) in the UK.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Prolapse Management
Relevance: 100%
-

Prolapse Types and Tips
Relevance: 72%
-

Pelvic health: prolapse
Relevance: 71%
-

Pelvic health: prolapse
Relevance: 70%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 66%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 65%
-

How to manage type 2 diabetes
Relevance: 25%
-
Your pelvic health matters: insights from NHS clinicians
Relevance: 24%
-

Long COVID - Managing Breathlessness
Relevance: 24%
-

Is there a protocol for managing concussions in rugby?
Relevance: 24%
-

Can fiber help with weight management?
Relevance: 23%
-

Are there self-help strategies for managing health-related anxiety?
Relevance: 23%
-

Can fiber help with weight management?
Relevance: 23%
-

Managing Chronic Illness Within the Family
Relevance: 23%
-

How are food allergies managed in UK schools?
Relevance: 23%
-

Is Wegovy used for type 2 diabetes management?
Relevance: 22%
-

Understanding and Managing Respiratory Illnesses in Families
Relevance: 22%
-

Strategies for Managing Seasonal Affective Disorder
Relevance: 22%
-

Can lifestyle changes help manage ADHD?
Relevance: 22%
-

What is the role of pain management in treating whiplash?
Relevance: 22%
-

How can nut allergies be managed?
Relevance: 22%
-

Can stress management aid in menopause masking?
Relevance: 22%
-
What is the role of diet in managing heart failure?
Relevance: 22%
-

Can lifestyle changes help manage tinnitus?
Relevance: 22%
-

How are product recalls managed in the UK?
Relevance: 22%
-

Are there apps that help manage and reduce household bills?
Relevance: 22%
-
How can I manage pain after a C-section?
Relevance: 22%
-

Managing and treating your child's eczema
Relevance: 22%
-

What role do schools play in managing concussions?
Relevance: 22%
-

What are the qualifications of the staff managing virtual wards?
Relevance: 22%
-

Is there an NHS app for managing prostate cancer care?
Relevance: 22%
-

How do live-in caregivers manage their personal time?
Relevance: 21%
-

What is the role of potassium in managing blood pressure?
Relevance: 21%
-

Are there any NHS apps for managing menopause symptoms?
Relevance: 21%
-

What role do lifestyle changes play in managing psoriasis?
Relevance: 21%
-

Where can I find support for managing Type 2 Diabetes in the UK?
Relevance: 21%
-
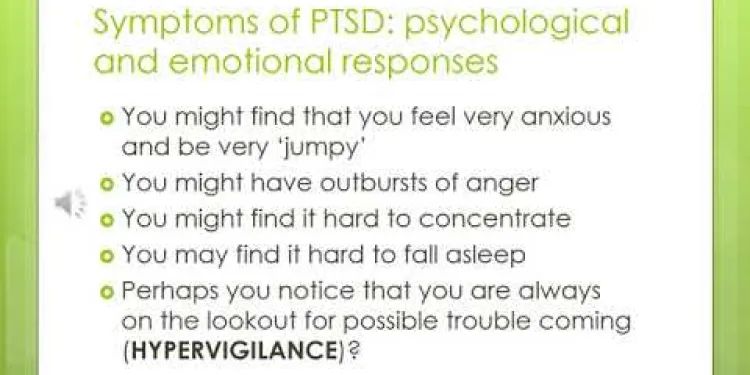
Understanding and Managing PTSD powerpoint slides with audio
Relevance: 21%
-

How important is the WHO for managing global pandemics?
Relevance: 21%
-

How can stress management affect cortisol levels?
Relevance: 21%
-

What role does diet play in managing obesity?
Relevance: 21%


