
Find Help
More Items From Ergsy search
-

Can flesh-eating disease occur after common surgical procedures?
Relevance: 100%
-
Is flesh-eating disease contagious?
Relevance: 68%
-

What is a flesh-eating disease?
Relevance: 66%
-
Can antibiotics alone cure flesh-eating disease?
Relevance: 64%
-

Can flesh-eating disease cause long-term complications?
Relevance: 64%
-
Can flesh-eating disease be treated?
Relevance: 62%
-

Who is at risk for flesh-eating disease?
Relevance: 62%
-

What causes flesh-eating disease?
Relevance: 61%
-

How does flesh-eating disease spread?
Relevance: 60%
-
What is the role of hyperbaric oxygen therapy in treating flesh-eating disease?
Relevance: 60%
-

How is flesh-eating disease diagnosed?
Relevance: 59%
-
What is the mortality rate for flesh-eating disease?
Relevance: 59%
-

Is surgery always required to treat flesh-eating disease?
Relevance: 59%
-
Can flesh-eating disease recur after treatment?
Relevance: 58%
-

What is the most common surgical procedure for BPH?
Relevance: 57%
-

Are there any preventative measures for flesh-eating disease?
Relevance: 56%
-

What is the difference between cellulitis and flesh-eating disease?
Relevance: 55%
-
What are the symptoms of flesh-eating disease?
Relevance: 54%
-

How quickly does flesh-eating disease progress?
Relevance: 51%
-

What is a flesh eating disease?
Relevance: 49%
-

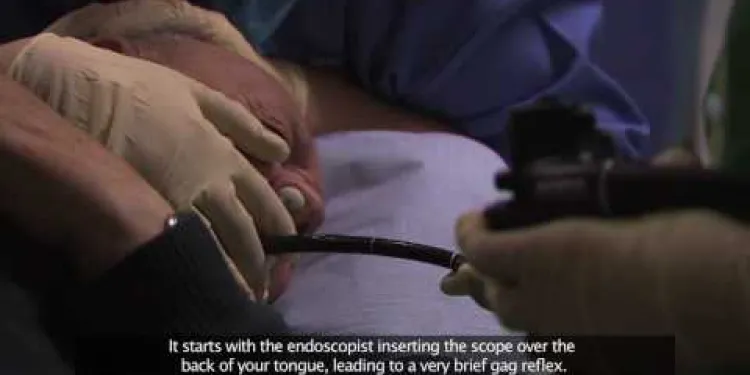
Bournemouth Digestive Diseases Centre: Endoscopy Procedure
Relevance: 41%
-
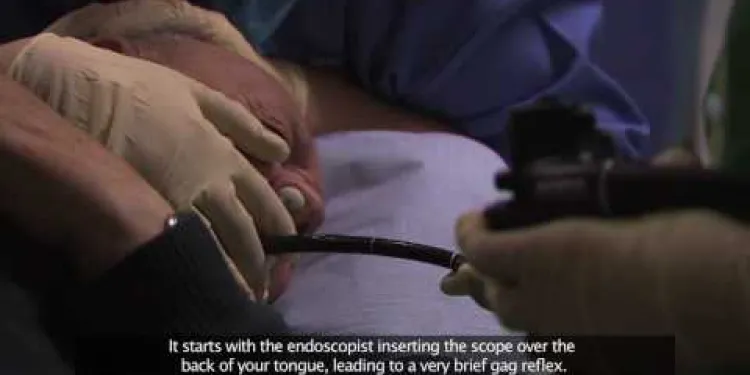
Bournemouth Digestive Diseases Centre: Gastroscopy Procedure (Subtitled)
Relevance: 37%
-

Is a C-section a common procedure in the UK?
Relevance: 36%
-

How can healthcare providers prevent the spread of flesh-eating bacteria in hospitals?
Relevance: 36%
-
Endoscopy Procedures | Colonoscopy
Relevance: 33%
-
Can a facelift be combined with other procedures?
Relevance: 30%
-
Having an operation or procedure at the Royal Free London
Relevance: 30%
-

Is surgery necessary for Crohn's disease?
Relevance: 30%
-
What is heart valve disease?
Relevance: 30%
-

Will I feel pain during the procedure?
Relevance: 29%
-

Liver disease | NHS
Relevance: 28%
-
What are minimally invasive procedures for BPH?
Relevance: 27%
-

Are there any complications associated with Crohn's disease?
Relevance: 27%
-
Thyroid eye disease. Squint surgery - The operation
Relevance: 26%
-
How does smoking affect Crohn's disease?
Relevance: 26%
-

What is the procedure for getting Turkey Teeth?
Relevance: 26%
-

What treatments are available for Crohn's disease?
Relevance: 26%
-

What is Parkinson's disease?
Relevance: 25%
-

Anaesthetic procedure for elective caesarean section (C section)
Relevance: 25%
-
How long does the Turkey Teeth procedure take?
Relevance: 25%
Understanding Flesh-Eating Disease
Flesh-eating disease, or necrotising fasciitis, is a rare but serious bacterial infection. It spreads quickly and can destroy skin, fat, and tissue covering muscles. The condition requires urgent medical care, often needing surgery and strong antibiotics.
While it is rare, the term "flesh-eating" is alarming, leading to significant public concern. Understanding its causes, symptoms, and risk factors is essential. Early diagnosis improves outcomes and recovery.
Risk Factors Associated with Surgical Procedures
Though rare, necrotising fasciitis can develop from surgical procedures. It usually enters the body through a break in the skin, such as a surgical incision.
Patients with weakened immune systems or chronic illnesses are more vulnerable. Conditions like diabetes, liver disease, or cancer raise the risk of post-surgery infections.
Poor wound care and hygiene can also increase the likelihood of infection. Following medical advice on wound care is crucial after surgery.
Symptoms to Watch For
Recognising the early signs of necrotising fasciitis is vital for quick action. Symptoms can appear within hours after a surgical procedure.
Initial signs may include severe pain, swelling, and redness at the surgical site. Fever and flu-like symptoms are also common.
If the condition progresses, the skin may turn purplish and blister. Seek immediate medical attention if these symptoms appear.
Preventing Post-Surgery Infections
Proper wound care is essential to prevent infections after surgery. Follow all post-operative care instructions from healthcare providers closely.
Ensure that the surgical wound is kept clean and dry. Regular monitoring for any signs of infection can aid in early detection.
Stay in touch with your healthcare team if there are concerns about your surgical site or symptoms. Early intervention can prevent severe complications.
Medical Response and Treatment
Prompt treatment is crucial for necrotising fasciitis. Surgery to remove infected tissue and intravenous antibiotics are the primary treatments.
If caught early, outcomes improve significantly. Medical professionals are trained to identify and manage these infections.
It's important to act quickly and not dismiss unusual symptoms following surgery. Swift medical response can be lifesaving.
Frequently Asked Questions
What is flesh-eating disease?
Flesh-eating disease, also known as necrotizing fasciitis, is a serious bacterial infection that destroys soft tissue.
Can flesh-eating disease occur after common surgical procedures?
Yes, although rare, flesh-eating disease can occur after surgical procedures if certain bacteria enter the body through surgical wounds.
What types of bacteria cause flesh-eating disease?
The most common bacteria causing necrotizing fasciitis are Group A Streptococcus, but others like Clostridium, and Vibrio vulnificus can also cause it.
How soon after surgery can necrotizing fasciitis develop?
It can develop within a few hours to several days after surgery.
What are the symptoms of necrotizing fasciitis?
Symptoms include severe pain, swelling, fever, and the skin may turn red or purplish. It can progress rapidly.
How is necrotizing fasciitis diagnosed?
Diagnosis is based on clinical examination, patient history, imaging tests, and laboratory tests.
How is necrotizing fasciitis treated?
Treatment involves prompt surgical removal of affected tissue, antibiotics, and supportive care.
Who is at risk for developing necrotizing fasciitis after surgery?
Individuals with weakened immune systems, chronic health conditions, or poor wound healing may be at higher risk.
How can the risk of necrotizing fasciitis be reduced after surgery?
Proper surgical techniques, hygienic practices, monitoring wounds, and treating any infections promptly can reduce risk.
Is necrotizing fasciitis contagious?
No, it is not spread from person to person.
How common is necrotizing fasciitis after surgery?
It is very rare, with only a small number of cases occurring relative to the number of surgical procedures performed.
What should patients do if they suspect necrotizing fasciitis post-surgery?
Seek immediate medical attention if there are signs of severe pain, rapid swelling, or discoloration near a surgical site.
Are there certain surgeries that pose a higher risk for necrotizing fasciitis?
Any surgery involving skin incisions could potentially lead to necrotizing fasciitis, but no specific surgery is particularly high risk.
What role does immune system health play in necrotizing fasciitis?
A robust immune system helps fight infections, so those with compromised immune systems may be more susceptible.
Can antibiotics prevent necrotizing fasciitis post-surgery?
While antibiotics can treat infections, they should not be used preventively without a doctor's guidance as they may not prevent the disease.
Can necrotizing fasciitis recur after treatment?
Recurrence is rare but possible, especially if there are underlying health issues or incomplete removal of infected tissue.
What is the mortality rate of necrotizing fasciitis?
The disease can be fatal if not treated promptly; mortality rates vary but are significant, underlining the need for swift treatment.
Can necrotizing fasciitis be mistaken for other post-surgical complications?
Yes, early symptoms can resemble other infections or complications. A medical assessment is critical for proper diagnosis.
What are the long-term impacts of necrotizing fasciitis?
Survivors may face long-term impacts including physical scarring, decreased mobility, and psychological trauma.
Are there any vaccines available for preventing flesh-eating disease?
Currently, there are no vaccines available specifically for necrotizing fasciitis.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Can flesh-eating disease occur after common surgical procedures?
Relevance: 100%
-
Is flesh-eating disease contagious?
Relevance: 68%
-

What is a flesh-eating disease?
Relevance: 66%
-
Can antibiotics alone cure flesh-eating disease?
Relevance: 64%
-

Can flesh-eating disease cause long-term complications?
Relevance: 64%
-
Can flesh-eating disease be treated?
Relevance: 62%
-

Who is at risk for flesh-eating disease?
Relevance: 62%
-

What causes flesh-eating disease?
Relevance: 61%
-

How does flesh-eating disease spread?
Relevance: 60%
-
What is the role of hyperbaric oxygen therapy in treating flesh-eating disease?
Relevance: 60%
-

How is flesh-eating disease diagnosed?
Relevance: 59%
-
What is the mortality rate for flesh-eating disease?
Relevance: 59%
-

Is surgery always required to treat flesh-eating disease?
Relevance: 59%
-
Can flesh-eating disease recur after treatment?
Relevance: 58%
-

What is the most common surgical procedure for BPH?
Relevance: 57%
-

Are there any preventative measures for flesh-eating disease?
Relevance: 56%
-

What is the difference between cellulitis and flesh-eating disease?
Relevance: 55%
-
What are the symptoms of flesh-eating disease?
Relevance: 54%
-

How quickly does flesh-eating disease progress?
Relevance: 51%
-

What is a flesh eating disease?
Relevance: 49%
-

Bournemouth Digestive Diseases Centre: Endoscopy Procedure
Relevance: 41%
-
Bournemouth Digestive Diseases Centre: Gastroscopy Procedure (Subtitled)
Relevance: 37%
-

Is a C-section a common procedure in the UK?
Relevance: 36%
-

How can healthcare providers prevent the spread of flesh-eating bacteria in hospitals?
Relevance: 36%
-
Endoscopy Procedures | Colonoscopy
Relevance: 33%
-
Can a facelift be combined with other procedures?
Relevance: 30%
-
Having an operation or procedure at the Royal Free London
Relevance: 30%
-

Is surgery necessary for Crohn's disease?
Relevance: 30%
-
What is heart valve disease?
Relevance: 30%
-

Will I feel pain during the procedure?
Relevance: 29%
-

Liver disease | NHS
Relevance: 28%
-
What are minimally invasive procedures for BPH?
Relevance: 27%
-

Are there any complications associated with Crohn's disease?
Relevance: 27%
-
Thyroid eye disease. Squint surgery - The operation
Relevance: 26%
-
How does smoking affect Crohn's disease?
Relevance: 26%
-

What is the procedure for getting Turkey Teeth?
Relevance: 26%
-

What treatments are available for Crohn's disease?
Relevance: 26%
-

What is Parkinson's disease?
Relevance: 25%
-

Anaesthetic procedure for elective caesarean section (C section)
Relevance: 25%
-
How long does the Turkey Teeth procedure take?
Relevance: 25%


